-
Definition
+Fractures of Acetabulum & Pelvis:
Fractures of the pelvis and acetabulum are among the most serious injuries treated by orthopedic surgeons. Often the result of a traumatic incident such as a motor vehicle accident or a bad fall, these fractures require rapid and precise treatment and, in some cases, one or more surgical procedures. People of all ages are vulnerable to these injuries. In addition, some elderly patients with fragile bones due to osteoporosis develop pelvic fractures and fractures of the acetabulum with a lower impact fall.
 Radiograph of a normal pelvis the complex nature of these fractures can be better understood by looking at the anatomy that is involved. The pelvis is made up of several bones (ileum, ischium and pubic bones) which create a bony ring, meeting at the pubic symphysis in the front and the sacrum (a bone situated at the lower end of the spine) in the back. Together with a number of ligaments and muscles, the bones of the pelvis support the weight of the upper body and rest on the hip joints. The pelvis protects abdominal organs including the intestines and the bladder, as well as major nerves and blood vessels. Pelvic fractures may occur at any location on the bones depending on the nature of the accident and the areas of impact.
Radiograph of a normal pelvis the complex nature of these fractures can be better understood by looking at the anatomy that is involved. The pelvis is made up of several bones (ileum, ischium and pubic bones) which create a bony ring, meeting at the pubic symphysis in the front and the sacrum (a bone situated at the lower end of the spine) in the back. Together with a number of ligaments and muscles, the bones of the pelvis support the weight of the upper body and rest on the hip joints. The pelvis protects abdominal organs including the intestines and the bladder, as well as major nerves and blood vessels. Pelvic fractures may occur at any location on the bones depending on the nature of the accident and the areas of impact.Radiograph of the pelvis demonstrating a fracture of the pubic bone
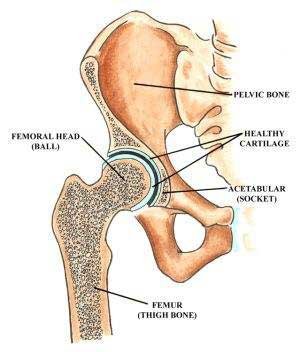
The acetabulum refers to the part of the pelvis that meets the upper end of the thighbone (the femoral head) to form the hip joint. In a healthy hip, these two bones fit together like a ball and cup, in which the ball rotates freely in the cup. Cartilage lines the bones where they meet at the joint and there is little friction between the surfaces during movement.
Anatomical illustration of the acetabulum
 The term broken hip usually refers to a fracture of the ball portion of this joint, that is, the upper femur, femoral neck or the femoral head. (See Hip Fracture for more on this injury.) In this section, we are speaking specifically of a fracture of the cup or acetabulum. Fractures of the acetabulum are harder to treat because access to this bone is more difficult, and because of the acetabulum's proximity to the major blood vessels to the legs, the sciatic nerve (the major nerve that arises from the lower spine and provides sensation and movement to the leg and foot), the intestines, the ureter and the bladder. Unlike a hip fracture, which can be treated relatively easily, to repair an acetabular fracture, the orthopedic surgeon, must, in essence, fix the broken bones from the inside out.
The term broken hip usually refers to a fracture of the ball portion of this joint, that is, the upper femur, femoral neck or the femoral head. (See Hip Fracture for more on this injury.) In this section, we are speaking specifically of a fracture of the cup or acetabulum. Fractures of the acetabulum are harder to treat because access to this bone is more difficult, and because of the acetabulum's proximity to the major blood vessels to the legs, the sciatic nerve (the major nerve that arises from the lower spine and provides sensation and movement to the leg and foot), the intestines, the ureter and the bladder. Unlike a hip fracture, which can be treated relatively easily, to repair an acetabular fracture, the orthopedic surgeon, must, in essence, fix the broken bones from the inside out.In fractures of this type, the femoral head is often driven through the acetabulum because of the impact of the fall or accident. If the femoral head ends up outside the acetabulum, this is known as a dislocation of the hip joint. Some patients have both a fracture and a dislocation.
Radiograph of the left hip demonstrating a posterior dislocation of the hip with an associated Posterior Wall type fracture of the acetabulum
Unfortunately, patients with fractures of the pelvis and/or acetabulum, also experiences serious injury to surrounding soft tissue (skin and muscles) and neurovascular structures (nerves, arteries and veins). In addition, especially in the case of pelvic fractures, adjacent organs can be seriously injured. With both types of fracture, there is significant bleeding and risk of nerve damage.
 In patients with multiple injuries, treatment begins with the trauma team at the scene, and then subsequently in the emergency room--a team of general surgeons, anesthesiologists and nurses--who work together to control bleeding, address damage to the head and chest, and other organs that may have been affected, such as the bladder and intestines, and to stabilize broken bones. During this early resuscitation phase of treatment, the orthopedic surgeon may need to stabilize the fracture by using an external frame to temporarily hold the bones in proper alignment while other problems are treated. This is called temporary external fixation. Surgeons construct these frames using steel pins that are inserted into the bone and joined together by clamps and rods and can do so very rapidly.
In patients with multiple injuries, treatment begins with the trauma team at the scene, and then subsequently in the emergency room--a team of general surgeons, anesthesiologists and nurses--who work together to control bleeding, address damage to the head and chest, and other organs that may have been affected, such as the bladder and intestines, and to stabilize broken bones. During this early resuscitation phase of treatment, the orthopedic surgeon may need to stabilize the fracture by using an external frame to temporarily hold the bones in proper alignment while other problems are treated. This is called temporary external fixation. Surgeons construct these frames using steel pins that are inserted into the bone and joined together by clamps and rods and can do so very rapidly.Radiograph of the pelvis demonstrating application of a pelvic external fixator.
Once the patient is stabilized--bleeding has stopped and other life-threatening injuries have been addressed--the fractures can be treated definitively. Successful treatment for both of these types of fractures requires the skills of an interdisciplinary team, with orthopedic surgeons working closely with the trauma team (general surgeons), the anesthesiologists and nurses. Following surgery, rehabilitation specialists play a key role in recovery.
Because of the complex nature of these fractures and because many orthopedic surgeons do not regularly treat them, patients who initially go to a community hospital for emergency attention are often transferred to an institution that specializes in such injuries.
-
Associated Injuries
+Contents will be available soon....
-
Immediate Management
+Abstract Operative management of displaced acetabular fractures yields better results than no operative management. Over the past decade, surgical approaches to the acetabulum and the surgical tactic for repair of common fracture patterns have been advanced. Excellent outcomes after repair of these injuries can be achieved. In some cases, as in the elderly, or in those cases in which there is significant destruction of the articular cartilage, primary total hip arthroplasty may provide the best solution. Removal of the femoral head allows for excellent exposure of the acetabulum, making it possible to stabilize most fractures without the need for extensile or intrapelvic approaches.
The surgical technique that has been successfully used calls for gaining primary stability of the acetabular columns by open reduction and internal fixation and then using the acetabular component to replace the articular surface. The columns need not be anatomically reduced. Multiholed acetabular shells can be used as internal fixation devices by placing screws into the columns enhancing the stability of the repair. In older individuals with severe osteoporosis, a typical fracture pattern results in intrapelvic dislocation of the femoral head with a blowout fracture of the anterior column and medial wall. Reinforcement rings with cemented acetabular fixation can be used in these cases. The femoral head can be used as bulk bone graft to replace and reinforce the reconstruction. Techniques common to revision of failed acetabular components are helpful in this setting. The results of reconstruction of severe acetabular fractures with total hip replacement have been reported to be similar to those achieved for reconstruction of osteoarthritis.
-
Definite Management
+Contents will be available soon....
-
Post Operative Period
+Following surgery, managing the patient's pain and managing any complications that arise due to the injury are primary concerns.
Initially, pain medication will be given by injection. However, many patients are able to use a pump that controls the amount of pain medication given. This is known as Patient Controlled Analgesia (PCA) and offers patients the benefits of managing his or her pain. Since there is a maximum dose that can be delivered at any given time, there is no danger that the patient will receive too much medication.
Other medications that may be given include anticoagulants to thin the blood and avoid the development of blood clots, which prevents bone formation in areas around the muscles.
Patients are encouraged to get up and out of bed as soon as possible, since doing so helps to avoid some of the complications associated with these injuries. A regimen of physical therapy is followed to maintain muscle strength and range of motion during recovery.
After surgery to repair a pelvic fracture or fracture of the acetabulum, many patients continue to feel the effects of damage to nerves that might have occurred during the traumatic event or the surgery. Important branches of the lumbar and sacral nerves may be either stretched or torn, especially in the case of unstable pelvic fractures. Injuries to the nerves result in decreased feeling in a limb and/or difficulty or inability in moving part of the limb. It is difficult to predict whether these nerves will fully recover. However, the majority of patients do regain some sensation and function of the limb within six to eighteen months after their injury.
-
Complications
+Throughout treatment and recovery, doctors and nurses are watchful for the following potential complications:
- Deep Vein Thrombosis and Pulmonary Embolism: Blood clots that may form in the veins of the pelvis, thighs, and/or lower legs and may travel to the lungs.
- Pneumonia: An infection of the lungs that may affect any patient who is confined to bed and cannot expand his or her lungs as fully as they normally do.
- Skin Problems resulting from being in one position for a long period of time.
- Muscle Complications due to inactivity.
- Heterotopic Ossification, a condition in which the body mistakenly forms bone in an area where there is normally muscle; prompt treatment is required to prevent this new bone from interfering with joint movement.
- Damage to the Head of the Femur: if the articular cartilage lining of the joint is affected in an injury to the pelvis, and particularly in fractures of the acetabulum, it's important to keep the surfaces of the joint from rubbing together-and to avoid the risk of future development of arthritis. Preoperatively, traction or a system of ropes, pulleys and weights are used to relieve pressure in the joint. Obviously, surgery with open reduction and internal fixation is performed to realign the joint with enough stability to allow immediate mobilization and hence preserve the smooth lining of cartilage and avoid subsequent arthritis. Avascular Necrosis of the Head of the Femur: Patients with a dislocated hip and/or fracture of the acetabulum may have disrupted blood flow to the head of the femur (the ball in the hip joint). This can result in death and collapse of bone tissue and hip joint arthritis.
- Nutritional Problems: The body requires more protein and calories during healing.
- Constipation resulting from inactivity
- Infection at the site of the injury
Patients who have suffered a traumatic accident or injury may experience psychological distress over changes in their appearance and physical functioning. The shock of becoming an accident victim may also linger. As with a serious illness, the patient may wonder "why me" and be searching for reasons the accident occurred. Difficulty sleeping and coping with the pain associated with recovery are very common. Patients with pre-traumatic depression or experiencing other stressful life events are more prone to experience psychological difficulty connected with their fracture.
In many cases, the passage of time eases these symptoms. At HSS, patients and their families have telephone access to trauma nurses with extensive experience in this field. Often they are able to address the questions and concerns that arise. When necessary, the patient's physician may recommend contact with a social worker or psychologist.
The common complications of surgery for the acetabular fractures are:
- Traction injury to the sciatic nerve
- Wound hematoma
- Wound infection
- Intra articular implants
- Heterotrophic ossification
- Avascular necrosis of head of femur and of fracture fragments
- Protrusio acetabuli
- Early degenerative arthrosis
- Implant loosening
-
FAQ
+Q. Why should I have the surgery?
A. If your surgeon recommends surgery it is because you have a displaced fracture and there is an incongruity in the acetabulum. Normally the acetabulum is a smooth cup, congruent with the femoral head, allowing for frictionless motion of the femoral head. If the fracture heals in the displaced position and there is a "step off" then the cartilage on the femoral head will wear away causing posttraumatic arthritis. This is painful, can be very debilitating, and possibly may lead to a hip fusion or total hip replacement. The goal of the surgery is to:
- Restore the normal shape of the acetabulum
- Decrease pain and allow for early ambulatory function
- Decrease the chance of post-traumatic arthritis
- Delay or avoid the necessity for a total hip replacement
Q. How long will I be in The Hospital for Special Surgery?
A. The typical inpatient stay for acetabular fracture surgery is 7-10 days.
Q. Will I have a brace or cast after surgery?
A. No. The fracture is reduced and stabilized internally with plates and screws.
Q. Will I have a limp after the surgery?
A. Most patients that undergo aggressive rehabilitation to restore muscle strength and flexibility do not have an abnormal gait.
Q. When do my sutures or staples come out?
A. The patient returns to the surgeon for a post-operative check-up after Ten to fourteen days of surgery. At this time, the wound is examined and the sutures or staples are removed. The patient may shower or bathe after they are removed.
Q. Do I have to go to a rehabilitation facility after my stay at The Hospital for Special Surgery?
A. No. Most of our patients do return home after their surgery. Physical therapy in the hospital insures that each patient is independent on a walker or crutches and is able to manage stairs. However, there are certain situations where a patient prefers to go to a rehabilitation facility post-operatively and this can be worked out in the hospital with the trauma social worker.
Q. When can I return to work?
A. Typically patients, with these injuries who do manual labor are on temporary disability for 6-9 months following surgery. Those individuals that have jobs that are physically less demanding, ie. Desk jobs return to work much earlier (some even after a few weeks). However, each case is evaluated on an individual basis.
Q. How much pain will I be in after surgery?
A. Pain is very subjective, however, at HSS, a complaint of pain is taken very seriously and every effort is made to adequately control the pain. Most patients do go home with oral medication.
Q. How long do I need to go to physical therapy?
A. Strengthening and flexibility exercises are very important components of the rehabilitative process. Most of the exercises necessary to increase strength such as running on the treadmill and or using the stationary bicycle do not commence until full weight bearing at 8 weeks. Most patients will continue with physical therapy for 6-12 months after surgery.
Q. How long will I be under the care of my surgeon?
A. Initially you will see your surgeon every couple of weeks and have conventional radiographs. At about 6 months you will return approximately every 3 months for x-rays followed by annual check-ups. Additional visits are unnecessary unless a problem arises.
Q. Is there any medication I can take or anything I can do to expedite the healing process?
A. No. A fractured bone typically takes 8 weeks to heal. There is no medication to speed up the healing. A healthy diet and adequate sleep are always recommended. Of note, smoking has been known to delay healing and sometimes arrest healing all together.
Q. My family member was brought to the hospital today with a fracture of the acetabulum, but we were told that surgery to repair the broken bone won't take place for at least a week even though she doesn't have other injuries. Shouldn't she be treated right away?
A. This delay will actually protect your relative. A fracture of the acetabulum is accompanied by a significant amount of bleeding. Over the course of the next 3-5 days bleeding will stop with the help of the body's own clotting mechanisms. Only after this happens is it safe to proceed with surgery.
Q.I will be undergoing repeat surgery for a pelvic fracture that happened 3 years ago. What are my chances for improved function and good recovery?
A. Unfortunately, there's no precise answer to this question. The success of the surgery depends on the potential for improving the alignment of the broken bones, your overall health, and ability to adhere to a rehabilitative program. While it is always easier to get good results with an initial repair of a fracture, previous surgery does not necessarily mean that you will not experience significant improvement.
Q. Why is it sometimes necessary to have more than one operation to fix a pelvic fracture? Can't the surgeon fix everything at once?
A. In many cases, the surgeon must approach the pelvic bones from different directions in order to complete the repair. Each of these approaches can require a separate surgery.
Q. I understand that I will have to start taking a blood-thinning drug before undergoing surgery for an acetabular fracture. Will that put me at greater risk for excessive bleeding?
A. Your physician has prescribed this medication for you to guard against the development of a blood clot in the veins of your pelvis, thighs or lower legs. Should such a clot develop and travel to your lungs, it can interfere with breathing and pose a significant danger. You will be taking a very low dose of this medication and will be watched carefully to ensure that no excess bleeding occurs.
Q.My grandmother broke her acetabulum after a simple fall in her home. How could this happen?
A. Your grandmother probably has osteoporosis, a condition in which the bone density decreases and the bones become more fragile and likely to break on impact. If she has not been assessed for this condition before, her physician will certainly do so and recommend a course of treatment to help prevent future fractures.

Dr. Rakesh Rajput
MBBS (Cal), MS Orth (Cal), FRCS (Glasgow)
MCh Orth (UK), FRCS Trauma & Orth (UK)
Director and HOD, Dept. of Orthopedics CMRI Hospital, Kolkata President AOPAS Specialist in Total Knee Replacement, Hip Replacement, Joint Replacement, Arthritis, Arthroscopy, Pelvic & Acetabular Trauma |









